ACCRA, Sept 15 (The African Portal) – The Chief Executive of Ghana’s National Health Insurance Authority (NHIA), Dr. Victor Asare Bampoe, has cautioned that fraudulent claims and illegal charges under the National Health Insurance Scheme (NHIS) risk delaying and derailing the smooth implementation of the reviewed NHIS service tariff regime.
He therefore called for stronger collaboration among stakeholders in the health sector, particularly the Ghana Health Service (GHS), to curb these practices, noting that they pose a major threat to the sustainability and efficiency of the Scheme.
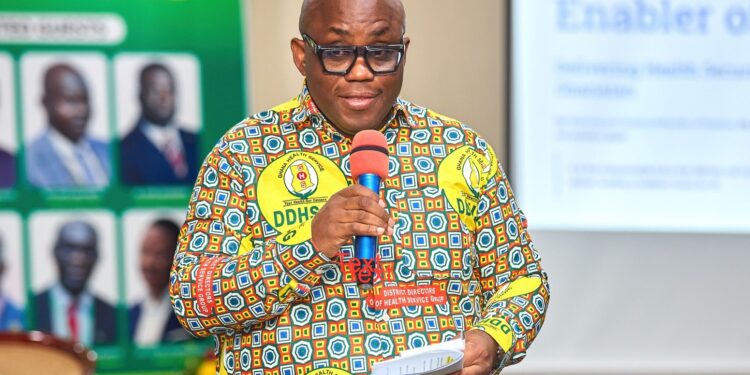
Dr. Bampoe made the remarks when he addressed the 32nd Annual Conference of Deputy Directors of Health of the Ghana Health Service in Kumasi last Friday, where he was a Special Guest of Honour.
According to him, while the service tariff has been reviewed and is ready for implementation, introducing it prematurely without addressing systemic loopholes would be tantamount to “pouring water into a basket.”
“The tariff adjustment is ready, but the system needs a thorough overhaul. We must eliminate leakages to ensure that what we pay as claims is truly for its intended purpose,” Dr. Bampoe cautioned.
Zero Outstanding Claims, Sustained Reimbursements
The NHIA Chief Executive revealed that the Authority has cleared all outstanding arrears dating as far back as 2018. He expressed gratitude to the government for uncapping the National Health Insurance Levy, which he said had facilitated the prompt payment regime introduced by the current executive management.
“Currently, there are no vetted claims on my desk awaiting approval. We are debt-free, and payments are now made monthly. If anyone is owed, it may be due to peculiar challenges, and our doors are always open,” he assured.
He credited the uncapping of the National Health Insurance Levy (NHIL) and the Ministry of Finance’s decision to release funds directly to the Authority, bypassing the Consolidated Fund, for ensuring timely reimbursements.
Illegal Charges and Fraudulent Claims
Dr. Bampoe, however, expressed worry over the persistence of illegal out-of-pocket charges, often wrongfully referred to as co-payments, as well as fraudulent claims by some providers.
“These practices undermine the Scheme and erode public confidence. Out-of-pocket charges for services already covered under the NHIS benefit package are illegal, not co-payments, and we must work together to end them,” he emphasised, citing the recent case at the Akim Oda Government Hospital as an example of the NHIA’s zero-tolerance policy.
He added that while most providers are professional and dedicated, a “few bad nuts” exploit the system at the expense of members and taxpayers.
Dr. Bampoe underscored that safeguarding the Scheme is a shared responsibility, calling on the GHS, NHIS’s largest service provider, to work closely with the Authority to end fraudulent practices.
“This is why when we talk about national health insurance, we always refer to the golden tripod: you, the providers; we, the financiers; and most importantly, the people we serve,” he noted.
He explained that striking a balance among these three pillars is critical to advancing Ghana’s Universal Health Coverage (UHC) agenda.
NHIS Performance and Policy Outlook
Highlighting recent performance, Dr. Bampoe disclosed that the NHIS covered about 18 million people in 2024, representing 56 percent of the national population. This year, coverage has already reached close to 20 million people, with a projection to exceed last year’s figures.
He added that the Scheme currently covers 95 percent of all disease conditions and is leveraging innovations such as the *929# renewal code and the MyNHIS App to expand access.
Looking ahead, he reaffirmed the Authority’s commitment to ensuring efficiency, transparency, and value for money in all its operations. He also emphasized that upcoming policy initiatives—including the Free Primary Health Care for All programme and the Ghana Medical Trust Fund (popularly known as Mahama Cares)—will complement the NHIS to provide end-to-end healthcare coverage without financial barriers.
“Together, with the reforms we are undertaking and the shared commitment of all stakeholders, the NHIS will continue to protect Ghanaians from catastrophic healthcare costs while driving us closer to achieving Universal Health Coverage,” Dr. Bampoe said.